Arthritis
Ankylosing Spondylitis
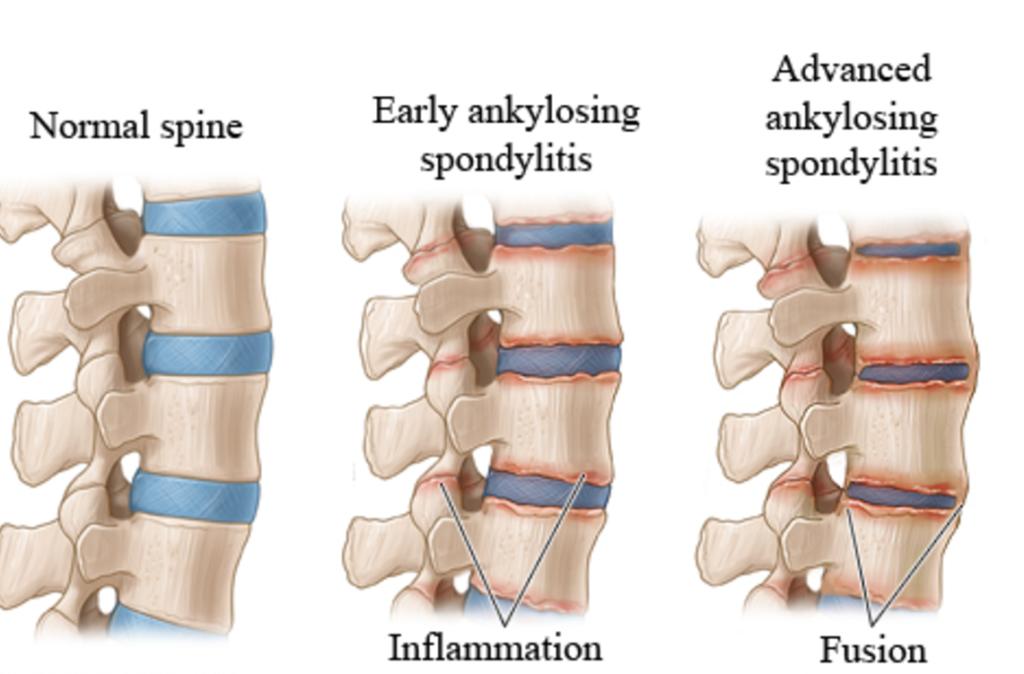
Ankylosing spondylitis is a type of arthritis that primarily affects the spine. The disease is characterized by inflammation and resulting stiffness and pain in the joints along the spine. The knee and shoulder joints may also be affected.
With ankylosing spondylitis the inflammation in the joints of the spine will typically result in parts of the vertebrae and joints in the spine fusing together. As parts of the vertebrae grow (or “fuse”) together, the spine becomes more rigid and inflexible.
The fusion takes place as a reaction to inflammation of ligaments or tendons at the site of attachment to bone. The inflammation causes bone to erode at the site of the attachment, and then as the inflammation subsides, the body’s natural healing process causes new bone growths in its place.
Because this new bone is stiff, as opposed to the elastic quality of the tissue or ligaments, the normal range of motion of the spine is diminished.
Ankylosing spondylitis most commonly is diagnosed in young men between the ages of 15 and 30, although it can affect anyone. Almost everyone with ankylosing spondylitis carries a specific gene called HLA-B27.
Bone Spurs (Osteophytes) and Back Pain
Bone spurs are a common finding in imaging tests, especially for people over age 50. Many patients are told that they have bone spurs in their back or neck, with the implication that the bone spurs are the cause of their back pain. While bone spurs may cause pain, many do not and it is important to receive an accurate clinical diagnosis for the underlying cause of the pain in order to form an effective treatment plan.
How Spinal Bone Spurs Can Cause Back Pain
Bone spurs typically cause back pain one of three ways:
Joint inflammation. Bone spurs of the joints of the spine (facet joints) can cause adjacent vertebrae to grind against each other, resulting in friction and inflammation. The inflammation can lead to pain, stiffness, and other symptoms.
Compression of a nerve root. The development of bone spurs can cause narrowing of the neural foramina, where the nerve roots exit the spinal column. With less space, the nerve roots may become compressed. Nerve root compression can cause paresthesia (tingling) if they become compressed. If the nerve root becomes inflamed, pain may occur.
Compression of the spinal cord. Bone spurs can grow into the spinal canal, where the spinal cord travels, leaving less space for the spinal cord. Compression of the spinal cord can cause weakness, strength loss, pain and other symptoms.When bone spurs cause a space in the spine to narrow, it is called stenosis. People who experience a compressed nerve root or spinal stenosis due to bone spurs are typically in their 60s and 70s.
Back or neck pain is common when the spine’s facet joints are inflamed or when the spinal cord or nerve roots are irritated. This inflammation and irritation can be caused by bone spurs.
Clinical Symptoms of Bone Spurs
The symptoms related to bone spurs typically:
- Develop slowly over time
- Become worse with activity
- Improve with rest
The specific symptoms a person feels depends on the location of the bone spurs.
Bone Spurs in the Neck (Cervical Spine)
Depending on the location of bone spurs in the neck, people may notice:
- Dull, achy pain in the neck that gets better with rest
- Radiating pain into one or both shoulders
- Pain, numbness, or tingling in one or both arms
- Weakness in the upper limbs
- Headaches that originate with a dull ache at the back or one side of the neck and travel up the back of the head
Numbness, tingling, and weakness in both shoulders, arms, and/or hands may be signs of spinal stenosis, commonly caused by bone spurs
Bone Spur Causes
Bone spurs are commonly associated with the normal aging process—everyone’s spine undergoes changes with age. Bone spurs can also develop as the result of a spinal condition, typically either spinal osteoarthritis or a degenerated disc.
Spinal osteoarthritis occurs with degeneration of any bony part of the vertebral column, commonly in the facet joints.
Each vertebra has two sets of facets located in the back of the spine. These facets meet with the facets of the vertebrae located above and below, forming facet joints. The facets move against one another during spinal movement.
For example, the facets are normally coated by smooth, slippery cartilage, so they glide against one another. When the protective layer of cartilage wears away, spinal osteoarthritis develops.
Spinal osteoarthritis causes:
Bone-on-bone friction at joint interfaces
Extra pressure on a spinal joint
In response to this added stress, bone spurs develop. Experts believe these bone spurs may be the body’s natural way to:
Re-distribute weight over a larger surface, protecting the bone1,2
Reduce range of motion, thereby discouraging movements that may cause bony stress
Spinal osteoarthritis most often affects the neck and lower back. It can cause stiffness, pain, and other symptoms. Symptoms are usually worse in the morning, get better after moving around, and then get worse again toward the end of the day.
Facet Joint Osteoarthritis
Osteoarthritis (degenerative arthritis) can cause breakdown of cartilage between the facet joints. When the joints move, the lack of the cartilage causes pain as well as loss of motion and stiffness.
The facet joints are located in the back portion (posterior) of the spine. The joints combine with the disc space to create a three-joint complex at each vertebral level. The facet joint consists of two opposing bony surfaces with cartilage between them and a capsule around it that produces fluid.
The combination of the cartilage and the fluid allows the joint to move with little friction. However, facet joint arthritis causes the cartilage to breakdown and the joint movement is associated with more friction. The patient loses motion and as they get stiffer they have more back pain.
Low Back Pain from Osteoarthritis
Typically, the low back pain is most pronounced first thing in the morning. Throughout the day, normal movement causes fluid to build up in the joint and it becomes better lubricated, which decreases the pain. Later in the day the pain typically becomes worse again as more stress is applied across the joint.
Conservative Treatments for Osteoarthritis
Conservative (nonsurgical) treatments that concentrate on maintaining motion in the back are most effective for relieving the pain.
- Stretching exercises for the hamstring muscles, hip joints, and the back can usually serve to prevent the pain from getting worse.
- For more severe pain, chiropractic manipulations can help relieve pain.
- Water therapy can be also be helpful since the joints are unweighted in the water and do not generate as much pain when being moved.
- NSAIDs
Surgery for Osteoarthritis
The only effective surgical treatment option for osteoarthritis is a fusion to stop the motion at the painful joint, but this surgery is generally not recommended since multiple vertebral levels tend to be affected by osteoarthritis and multilevel fusions are generally not advisable.
Rheumatoid Arthritis in the Spine
Rheumatoid arthritis is a disease that causes destruction of joints in the body. The disease can occur in any joint in the body and is most commonly symptomatic in the small joints in the hands and feet. When rheumatoid arthritis affects the joints in the spine, it is far more common for the neck (cervical spine) to be affected than for the lower back.
Rheumatoid Arthritis Symptoms in the Spine
Rheumatoid arthritis of the spine can lead to neck pain, back pain, and/or pain that radiates into the legs or arms. In advanced cases, the joint deterioration in the spine can lead to compression of the spinal cord and/or the spinal nerve roots.
The symptoms of rheumatoid arthritis in the spine are generally similar to the symptoms of osteoarthritis (also called degenerative arthritis). The range of symptoms is broad and can include any combination of the following:
- Pain is the most common symptom, especially pain at the base of the skull as rheumatoid arthritis most commonly affects the joints connected to the upper cervical vertebrae
- Swelling and warmth in one or more joints, may even be described as burning
- A feeling of local tenderness when the joint of the affected area of the spine is pressed
- Loss of flexibility of the joint(s) in the affected area of the spine
- A crunching feeling when the joint is moved (called crepitus), particularly notable in the neck (although this crunching also happens in normal joints)
- Headaches, related to cervical rheumatoid arthritis
- Pain that radiates down one or both arms, indicating that a cervical spinal nerve root is affected
- Pain that radiates down one or both legs, indicating that a lumbar nerve root is affected
- A change in the ability to walk can signal increasing pressure on the spinal cord.
- Sensations of tingling and/or weakness in the arms or legs, or a loss of coordination or ability to walk, which may be an indication that the spinal cord is affected.
- Any type of difficulty with bowel or bladder control, such as incontinence or inability to urinate, or lack of ability to control the bowels
Symptoms of bowel or bladder dysfunction or change in the ability to walk or move the arms are serious medical symptoms and immediate medical attention should be sought.
Rheumatoid Arthritis Treatment
The goals of treatment for rheumatoid arthritis in the spine are primarily to:
Reduce or eliminate the pain
Maintain the ability to function in everyday life
Reduce or slow the progression of the disease.
For the vast majority of people, treatment is nonsurgical and will include one or a combination of physical therapy and exercise, medications, diet and nutrition, and possibly alternative or complementary forms of care. Surgery for rheumatoid arthritis in the spine is rare.
